GI Surgery
By
Dr.Bipin Vibhute
What is a GI Surgery?
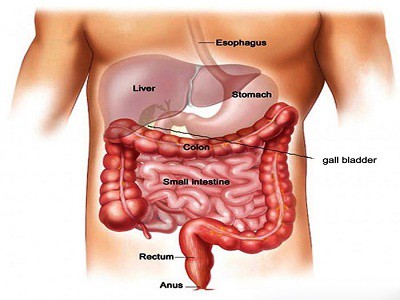
The treatment that aims to eradicate the diseases breeding in all the integral parts of our digestive system is known as gastrointestinal surgery. The body parts which are at risk of being infected with fatal diseases are the esophagus, stomach, small intestine, large intestine, and rectum (the hollow organs of the digestive system) as well as the liver, gallbladder, and pancreas (the solid organs of the digestive system).
Apart from the disorders that could impact the Gastrointestinal (GI) tract, it could be a cancerous or a noncancerous growth, a damaged part or even a hernia which could damage it.
GI Surgery guide
Skim through this guide blog that covers every important aspect of a GI Surgery in India.
1. Who is eligible for the GI Surgery?
Your eligibility will be decided based onwhether you have the following problems or not:
● Inflammatory bowel disease –
-When the immune system attacks the intestines and causes them to become inflamed
● Diverticular disease –
-When diverticula (small, inflamed and painful pouches in the large intestine) develop, the doctor may recommend bowel resection surgery
● GI bleeding
● Gallbladder disease –
-When the gallbladder must be removed using a surgical procedure known as cholecystectomy
● Gastro esophageal reflux disease (GERD) and Hiatal hernias –
-When acid reflux causes heartburn, it may be because of the Hiatal hernia (when the stomach pushes through the diaphragm). To resolve this problem, the surgeon will perform a fundoplication in which they will wrap the top of the stomach around the bottom of the esophagus so that the acid can be kept out.
● Hernia –
-When a body part belonging to the digestive system comes in contact with a weak spot in the wall of protective muscle or connective tissue
● Liver disorders
● Colorectal cancer
● Colon cancer
● Rectal prolapse –
-When the intestine comes through the anus
● Appendicitis –
-When the appendix becomes infected and inflamed, it may be removed using a surgery known as appendectomy
PLEASE NOTE: To remove the cancerous tumor, the surgeon may also have to remove other segments of the digestive system such as part of the pancreas, liver, or intestine with cancer.
2. How is GI Surgery performed?
There are multiple ways a general GI Surgery can be performed. But the type of surgery will depend on the patient’s condition.
Here are some of the most commonly implemented methods:
1. OPEN SURGERY:
Certainly quite invasive, this surgical procedure involves opening up the body using one cut. A scalpel and other tools are used to do so.
2. ENDOSCOPY:
This surgical procedure involves the doctor inserting a long, thin tube with a tiny camera to see the inside of the body through the nose, mouth or any other natural opening of the body. And, the surgery is conducted by inserting small instruments through the scope.
3. LAPAROSCOPY:
This surgical procedure involves a laparoscope (thin, flexible tube with a lighted camera) which is inserted through a small incision to perform the surgery. The surgeons may even insert small instruments through other small incisions to gain access to the site where treatment is needed.
4. ROBOTIC SURGERY:
This surgical procedure involves a computerized system in which the surgeon controls mechanical arms that are capable of holding a camera and the surgical instruments.
The surgeon may even take the assistance of a console that provides a high-definition, magnified 3D view of the surgical site.
The robotic arms have been known to perform much better than human arms because they tend to have a greater range of motion and more finesse when it comes to performing such procedures.
As you can observe, the three ways mentioned above are minimally-invasive and pro-modern technology, thus reducing the recovery time and the pain experienced by the patient.
The detailed visuals which the tiny camera projects helps the surgeons pinpoint the problem and put an end to it almost instantaneously and strategically.
Therefore, when your surgeon suggests one of the ways to conduct a GI-related surgery, don’t feel wary of the technological advancements involved.
3. What happens before the GI surgery?
Our advice is to listen to the advice given to you by the doctor and nurses before you show up for surgery.
We also recommend making some arrangements beforehand. These include:who will take care of you post-surgery? Whether your bathroom will need a grip bar for you to use or not? And, how will you manage to climb stairs in your house, if you have any?
Small arrangements such as these can help you paint the bigger picture of a speedier recovery.
4. What happens during the GI surgery?
Before the general anesthesia makes you unconscious for the entirety of your operation, you will be given specific instructions as to what you must eat before arriving at the hospital, when to stop eating and which medications to take right before the surgery.
Before it begins, an intravenous catheter (IV) will be inserted in your arm to administer medication.
Don’t worry. You will be asleep while the surgeon performs the procedure. Therefore, the phrase ‘pain intolerance’ should not upset you anymore.
When you have been sedated, the nursing staff will administer your health and notify the doctor instantly if they see you showing any signs of distress anytime during the operation.
5. What happens after the GI surgery?
The following ought to happen when you wake up from your general gastrointestinal surgery:
-Upon waking up, you will feel drowsy, tired and weak.
-A nurse will hand you some water but not any meals.
-You will receive pain medication orally and your catheters, as well as, tubes will be removed gradually.
-You will be asked to resume moving around. So, sitting up in a chair and going to the bathroom can be achieved. Nevertheless, someone from the hospital staff can help you walk.
-The doctor will visit you frequently so that they can administer your recovery, progress and order additional tests such as scans to confirm that you are indeed healing properly.
-The doctor or the nurse will coachyou and your caretakers on how to keep the incision clean and when to take your medication.
-The duration of your stay in the hospital after waking up from the surgery will depend on your condition. When the doctor deems your condition stable enough, you will be taken home.
6. Advanced Laparoscopic Procedures
1. Laparoscopy for achalasia cardia:
With esophageal achalasia being such a rare disease, laparoscopy as a minimally-invasive procedure decreases its mortality rate to a 0% as compared to the 1.2% mortality rate after open surgery. This disease is incurable but its symptoms can be decreased.
2. Laparoscopy for hiatus hernia:
A Hiatal hernia occurs when a part of the stomach moves upward and into the chest. To rectify this, a laparoscopic approach known as Nissen fundoplication in which the surgeon makes only a handful of incisions to the abdomen are involved. When compared to open surgery, this one is less painful and reduces the chances of infection.
3. Laparoscopy for hydatid cyst and liver cysts:
This surgical procedure aims to treat the hydatid cysts of the liver which entails evacuating the liver cyst content, preventing spillage, sterilizing the cavity and managing the residual cavity.
4. Laparoscopy for gastric cancer:
Because of this less intrusive surgical procedure, gastric cancer can be managed as laparoscopy can detect the metastasis and is highly helpful during the preoperative staging of the malignancy.
5. Laparoscopy for benign conditions of the esophagus:
When benign conditions of the esophagus take the form of large esophageal leiomyomas, a laparoscopic approach can be used to treat it because of its preference over open surgery or open thoracotomy. A malignant lesion of the esophagus is called an esophageal leiomyosarcoma.
6. Laparoscopy for the benign and malignant condition of the small and large intestine:
For people with small bowel tumors, a single-incision laparoscopic technique is advocated. However, when compared with conventional laparoscopy (LAP), the operation duration and the hospital stay remain the same.
7.Laparoscopy for right Hemicolectomy:
This is considered a safe option to treat cancers of the right colon. It allows the respective patient to resume their normal diets soon and their hospital stay is also considerably shorter than those spent after open surgery. However, mortality and morbidity rates remain the same for both approaches.
8. Adrenlactomy:
This surgery constitutes the removal of one or both of the adrenal glands. They are situated above our kidneys.
9. Spleenactomy:
The removal of the spleen by making an incision in the body is what constitutes this procedure.
10. Laparoscopy for rectal prolapse:
To control the prolapse, prevent constipation or impaired evacuation, laparoscopic surgery has been applied since the twentieth century. Whether it will be laparoscopic or open will depend on the patient’s condition and the surgeon’s preference.
11. Surgery for rectal cancer:
To remove early-stage rectal cancers in the lower rectum (the part closest to the anus), the surgeon will insert instruments through the rectum and cancer will be removed from the rectal wall.
Or, a transanal minimally invasive surgery (TAMIS) may be performed using standard laparoscopic equipment in which it will be inserted into the anus through a special port to remove early-stage cancer in the rectum.
12. STARR (Stapled Trans-rectal Resection):
To correct anatomical defects such as distal intra-rectal intussusceptions, a rectocele, and obstructive defecation syndrome, this safe procedure was introduced in the UK not too long ago.
As you can tell, the above procedures can either be exclusively laparoscopic gastrointestinal surgery procedures or open procedures. Sometimes, the surgeons will have the opportunity to choose between the two or they may only have to stick with the one which is most necessary and provides more promising outcomes.
7. Cost of GI surgery
Gastrointestinal surgery cost in India can go up to Rs. 5 Lakh rupees. The cost can increase due to factors such as the expensive and high-tech instruments required during the surgery and the costly medicine needed after it.
8. Care after GI surgery
The predominant instruction which will be given to you by your transplant surgeon before being discharged is that you do not over-exert yourself and that you rest as much as possible.
There should always be a caretaker who can change your dressing on time and refill your medication when it is about to run out. So, make sure that such arrangements are put in place long before you go for your GI surgery.
At home, you should also be perceptive when confirming if your wound is healing well or not. If it is not, it is excessively important that you notify someone from your transplant team as soon as possible.
9. What are the complications and risks of GI surgery?
GI surgery complications will be many, considering it is comprised of so many other fragile surgeries. The risks associated with it are:
● Bile leakage
● Organ failure after severe sepsis and septic shock
● Intra-abdominal bleeding
● Mechanical small bowel obstruction (SBO)
● Localized or generalized peritonitis
● Wound infection
● Pneumonia
● Urinary retention
● Urinary tract infection (UTI)
● Deep venous thrombosis (DVT)
● Pulmonary embolism (PE)
Knowing about the number of GI surgery risks can be scary for most patients. However, if your surgery specialist hosts the ability to think on their feet and have plenty of experience in GI transplant surgeries, then the mortality rate can be brought down drastically.
10. How to choose a transplant centre ?
Choosing a transplant centre can either depend on your general health physician’s recommendation or your insurance policy’s guidelines. Nevertheless, here are some quick parameters to keep in mind when choosing the right transplant centre for GI surgery:
● The annual report disclosing the number and type of transplants done
● Whether the transplant centre has a multidisciplinary approach to the GI surgery complications or not
● Whether it has the latest medical technology and infrastructure
● Online reviews and experiences of past patients
● Provision of endoscopic and laparoscopic procedures
11. Results of GI surgery
GI surgery survival rates
The survival rates will depend on the patient, their disease, the mode of treatment and the transplant centre chosen.Other factors that cannot be overlooked when measuring survival rates are the patient’s history, their medical condition before the surgery and the surgeon’s level of expertise.
Some predictors of a failed GI surgery are comorbidity (overlap of different medical conditions), type of operation, blood loss, and re-operation.
Despite that, if we had to ballpark it, the GI surgery mortality rate is 2.5% or lower.
One must still have some faith in the long strides medical science has taken today. Therefore, an in-depth conversation with your surgeon about the course of your operation should take place before proceeding.
12. Diet and nutrition after GI surgery
An experienced nutritionist from the transplant team will help you at every stage of planning out your diet post-GI-surgery.
They will advise you to chew slowly and eat food that resembles mashed potato consistency.
When it comes to fluids, not only water but also pudding, sherbet, ice cream as well as yoghurt can be consumed without any qualms.
It is completely normal to not feel hungry or not be able to eat enough protein that can promote wound healing. If this happens, you will be hooked to a feeding line called PICC (peripherally inserted central catheter).
Transplant Team
A liver transplant is an operation that involves the replacement of a patient's diseased liver with either a whole or partial healthy liver from a donor.


Dr. Aniruddha Bhosale
Consultant Liver & GI surgery

Dr. Apurv Deshpande
Liver and Multi Organ Transplant

Dr. Abhijit Mane
Asst Consultant Liver & Multiorgan Transplant

Dr. Manoj Raut
Consultant Liver Transplantation Anaesthesia & Critical Care

M/S. Malvika Karkare
Sr. Transplant Dietition
Transplant Team

Dr. Bipin Vibhute
Liver & Multiorgan Transplant Surgeon
A liver transplant is an operation that replaces a patient’s diseased liver with a whole or partial healthy operation that replaces.
Patient Reviews
Liver Transplant
Liver Transplant
“Dr. Bipin Vibhute sir performed liver resection surgery on my father Dr. explained all steps involved in the surgery, how surgery will be performed, precautions to be taken after surgery, recovery time etc. Dr. Bipin Vibhute sir and entire team is very cooperative, down to earth. They have taken good care of my father after surgery. Even entire team is available on Whatsapp to address our questions.
Abdullah Parkar,
(Transplant Year: 2022)
Read full story here
Liver Transplant
Liver Transplant
Organ Donation
Why we should Donate Organs?
By Dr.Bipin Vibhute
The biggest donation in this world is Organ Donation, by which we can save multiple lives. To save someone’s life is the biggest thing in this world. Being a donor is like having superpowers. By donating organs you give hope or a chance of living to a person who has left all the hopes of surviving.
Even if a person dies, his organs are not dead. The organs of a dead person will be of no use after the body is burnt or buried. But these organs can save up to eight lives if we donate them. We all understand the importance of Organ Donation, but how many of us support and wish to donate our organs.
Question & Answers
Blogs
Get moving and sit less for a healthy liver
Keeping active and exercising daily will aid in your overall health and the liver by minimizing fat accumulation and lowering your chances of obesity, type 2 diabetes,...
What is Portal Hypertension?
Our intestine stores nutrients that our bodies require when we eat or drink; along with these nutrients, it includes RBCs, WBCs, platelets, food, and hazardous...
What is a Liver Function Test?
What is a Liver Function Test? A liver function test is a blood test that examines the blood in a laboratory to assess the liver's general health and for liver damage....